How to register for the Provider Portal
The Delta Dental of Washington Provider Portal is a hub of resources to support your practice's experience, including member benefits and eligibility, processing policy, clinical guidelines, procedure code lookup, and more. Here, you'll also find information specific to your patients and your practice, including claims status and payment vouchers.
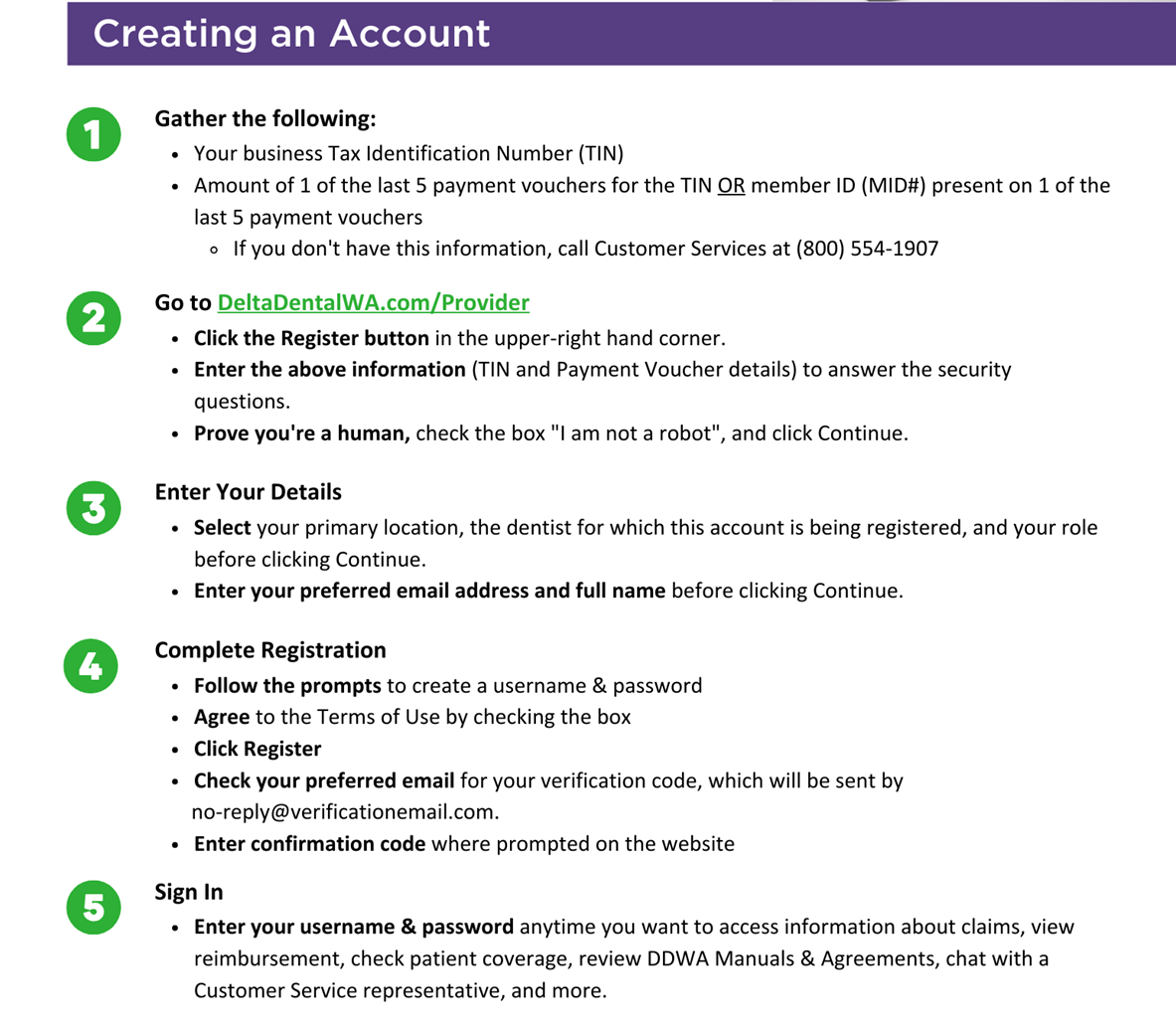
Use the following instructions to register, and view the Frequently Asked Questions below to learn how your new account can support your practice.