You want to take care of your oral health, but how do you do it without breaking the bank? One big factor to getting the most out of your dental benefits is to understand what goes into the cost of oral healthcare. Dental coverage plays a significant role in managing these costs, but deciphering the intricacies of coverage can be daunting. In this article, we'll delve into the components of dental insurance costs to help you navigate your way to optimal oral health without financial stress.
Dental insurance essentials
Submitted Charge: This is the starting point to any claims and out-of-pocket expenses. It is the amount your provider bills for a specific service before any adjustments or input from the benefits company.
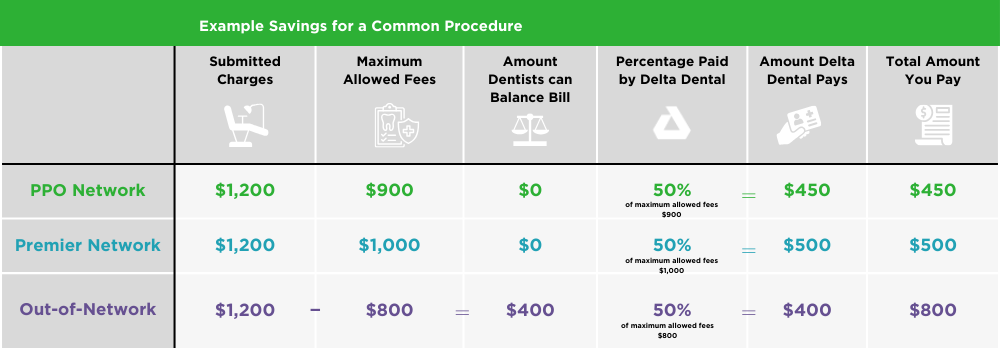
Maximum allowed fees: Also known as allowable charges, these are the highest amounts that benefit providers are willing to pay for specific dental services. Understanding these limits is crucial as they affect the coverage provided by insurance and the patient's out-of-pocket expense.
Balance billing: Balance billing is when a submitted charge is more than the maximum allowed fees, and your provider bills you for what your benefits don't cover. This practice can lead to additional out-of-pocket costs, particularly if the provider is out-of-network or charges exceed the maximum allowed fees. One of the benefits of being a Delta Dental of Washington benefits member is that our networks eliminate balance billing.
Percentage paid by dental provider: Some dental providers cover a portion of the total cost of services through discounts, insurance network participation, or other arrangements. Knowing the percentage covered by the provider can significantly impact the patient's financial burden.
Out-of-pocket costs: These include deductibles, copayments, coinsurance, and charges not covered by insurance. Understanding these expenses is crucial for effective budgeting and planning for dental care.
Copayment (Copay) and Deductible: Copay is the preset amount patients must pay before receiving a covered service, while the deductible is the amount paid directly to the dentist before insurance benefits kick in.
Annual maximum: This is the cap set by dental insurance plans on the total benefits paid by the benefit provider within a year. Once this limit is reached, coverage ceases until the next plan period.
Factors affecting costs
There are several factors that affect the cost of oral health coverage, like location, plan specifics, and the economy. Costs can fluctuate year-to-year. Here are just a few of the things that may affect how much you pay for coverage.
Geographic location: Costs can vary based on where you live due to differences in the cost of living and market dynamics.
Insurance plan specifics: Each insurance plan has unique coverage limits, networks, and reimbursement rates that influence costs.
Economy/workforce shortages: Economic factors and shortages in the dental workforce can impact costs and access to care.
Managing dental costs:
Maximizing Insurance Benefits: Using in-network providers can maximize coverage and reduce out-of-pocket expenses.
Utilize resources like MySmile: Delta Dental of Washington's MySmile platform and Find a Dentist tool can help you locate in-network providers and estimate costs.
Know before you go: Use Delta Dental of Washington's cost estimator to anticipate expenses for upcoming in-network dental services, empowering you to make informed decisions about your oral health care.
Understanding the components of dental insurance costs is crucial for effectively managing expenses and maintaining oral health. By familiarizing yourself with these factors and utilizing available resources, you can navigate the complexities of dental insurance with confidence, ensuring both your smile and your wallet stay healthy.


